5 Ways Strength Training Benefits your Pelvic Health
By Julia Rosenthal
Pelvic Health Physical Therapist
People suffering from pelvic pain are often told to avoid strength training to help alleviate a wide range of symptoms like pelvic pain, prolapse, incontinence, constipation and more. This messaging fosters an increased fear of movement, sense of disability, and overall decrease in a person’s ability to navigate their environment. Being able to load our bodies is an essential part of daily life. We load ourselves all the time when we’re holding a laundry basket, carrying groceries, picking stuff up off the floor, putting things away on a high shelf… the list goes on. Loading is inevitable, so we need to prepare ourselves for it. Plus, strength training has many physiological benefits that have a profound positive impact on pelvic health. Keep reading to learn five ways that a strength training program tailored to a person’s needs will improve rather than worsen their symptoms.
1. Training decreases musculoskeletal stress on the pelvic floor
 Your pelvic floor works with the rest of the muscles in your body, not in isolation. Building strength in the feet, hips, and trunk helps take some of the pressure off your pelvic floor muscles. How you go about this matters when you are suffering from pelvic pain or other forms of pelvic floor dysfunction.
Your pelvic floor works with the rest of the muscles in your body, not in isolation. Building strength in the feet, hips, and trunk helps take some of the pressure off your pelvic floor muscles. How you go about this matters when you are suffering from pelvic pain or other forms of pelvic floor dysfunction.
There are certain movement and breath patterns that may lead to exacerbation of pelvic floor symptoms. Addressing and re-educating those patterns is an important part of a good strength training program for a person with pelvic floor dysfunction. Some of those patterns include:
- Holding your breath (or doing so with a bad strategy where a breath hold is appropriate)
- Overly bracing your abs
- Overly squeezing your glutes or pelvic floor muscles
- Flaring the ribs and tipping the rib cage back
Realistically, even if you avoid lifting in the gym, you’ll need to squat to get in and out of a chair, hinge to get things off the floor, brace your trunk to carry heavy groceries, etc. That’s why it’s important to prepare your body for those tasks. It will increase your capacity to take such tasks on. Plus, it can be a lot of fun!
2. Training Increases nervous system resilience, internal safety, and sense of empowerment
Training is a form of stress. It has many physiological effects on the body, one of which is the release of cortisol (your stress hormone). Therefore, training can be a place to practice regulating the body in the face of stress, which carries over to stressors that you might encounter outside of training, and increases your capacity to navigate trauma-related triggers. Establishing these new neural pathways helps promote a feeling of safety in your own body.
The fact that training has the potential to raise cortisol levels is often a reason that people with pelvic pain are encouraged to avoid it. However, avoiding strength training is just cutting out a variable and not actually solving the problem – what happens when the world presents you with a stress that your body can’t handle? Strength training is an opportunity to introduce stress in an appropriately dosed way that gives your body an opportunity to learn how to manage stressors you may encounter. It can support nervous system flexibility by teaching the system how to shift between sympathetic (fight or flight) and parasympathetic (rest and digest) states.
Also, achieving gym goals and lifting heavy things can help establish a sense of power, confidence, and autonomy. This can translate into regular life outside the gym and foster a sense of empowerment.
3. Training produces metabolic benefits that help reduce the effects of chronic stress and regulate systemic inflammation
 The higher your exposure to different stressors – including both psychological/emotional stressors and physiological stressors such as lack of sleep, insufficient nutrient intake or absorption, digestive distress, and poor blood sugar regulation – the more inflammation will be present in the body. The presence of chronic, systemic inflammation contributes to chronic stress as well as persistent pain.
The higher your exposure to different stressors – including both psychological/emotional stressors and physiological stressors such as lack of sleep, insufficient nutrient intake or absorption, digestive distress, and poor blood sugar regulation – the more inflammation will be present in the body. The presence of chronic, systemic inflammation contributes to chronic stress as well as persistent pain.
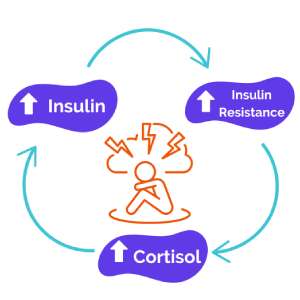
Building muscle helps curb chronic inflammation by decreasing insulin resistance. Insulin is the hormone that your body releases to help glucose (sugar) get into your cells so they can use it for energy. When your body faces chronic stress, your metabolism slows, and insulin becomes less effective at unlocking your cells so that they can receive and use the glucose in the bloodstream. When there is more glucose in the bloodstream than the body can use, it can get stored either as glycogen (another form of sugar) in your liver or your muscles, or it can be stored as a lipid (a fat) within adipose tissue (fat cells). Increasing adipose tissue mass can contribute to increased systemic inflammation. Increasing adipose tissue mass can also lead to an increase in estrogen production, contributing to estrogen dominance which can be a factor in multiple pelvic health conditions.
So how does building muscle help? Muscle helps increase your body’s sensitivity to insulin, meaning that your body gets better at using the glucose you get from the foods you eat, and less of that glucose gets stored in adipose cells. This leads to a decrease in adipose tissue mass and therefore a decrease in systemic inflammation.
Oftentimes, people with pelvic health conditions are told that losing weight is the solution. Unfortunately, the advice they are given is to increase cardiovascular exercise and decrease or even eliminate carbohydrate intake. This advice is problematic for multiple reasons given the physiology explained above. While doing appropriately dosed amounts of cardiovascular exercise has benefits, doing too much of it at too high of an intensity can drive significant increases in inflammation and cortisol. This, paired with under-eating, slows metabolism and increases insulin resistance, physiological stress, and systemic inflammation. Furthermore, taking out carbohydrates (aka sugars) completely is also just removing a variable rather than solving a problem that is happening on a cellular level, which is that the body is not responsive enough to insulin to use the sugars you ingest effectively.
All of this information may leave you wondering how you can strength train in a way that helps you build muscle without driving cortisol level increase in the body. The answer: a well constructed strength training program that introduces progressively more challenging lifts and heavier weights. These training sessions should have low enough repetitions that you can challenge yourself with heavier loads, adequate rest time between sets of exercises, and should only be programmed 2 – 3 times a week so that you have enough time to recover before your next training session.
4. Training improves sleep quality
Sleep is widely regarded as one of the most important aspects of healing and recovery. Resistance training helps the body produce a chemical called adenosine, which promotes sleep. Adenosine binds to cellular receptors, inhibiting neural activity and causing drowsiness. By increasing the production of adenosine, resistance training improves all aspects of sleep, especially sleep quality.
There are a lot of unknowns around the mechanisms by which resisted exercise affects your sleep, but we do know that strength training can improve symptoms of depression and anxiety, regulate body temperature, change your body’s energy expenditure, and relieve musculoskeletal pain, all of which have the potential to improve sleep.
4. Training improves your ability to manage large changes in intra-abdominal pressure
One of the more common sources of symptom provocation for people with pelvic floor issues is movements or activities that involve changes in intra-abdominal pressure. That includes things like sneezing, coughing, laughing, running, quick changes of direction, and jumping. Training can include movements that help prepare your body to better respond to those sorts of rapid pressure changes.
 Part of training this quality is learning to find coordination in the “core canister,” or the muscles that make up the deep control of the trunk including the diaphragm, deep abdominal muscles, small local muscles of the spine (the multifidi), and your pelvic floor muscles. One way that training can help your body achieve that coordination is to help you find the position where your ribcage is stacked over your pelvis. In that position, your diaphragm, trunk muscles, and pelvic floor muscles are best situated to work together to manage the downward pressure that happens both when you produce force (push your body away from the ground) and absorb force (control your body as it approaches the ground).
Part of training this quality is learning to find coordination in the “core canister,” or the muscles that make up the deep control of the trunk including the diaphragm, deep abdominal muscles, small local muscles of the spine (the multifidi), and your pelvic floor muscles. One way that training can help your body achieve that coordination is to help you find the position where your ribcage is stacked over your pelvis. In that position, your diaphragm, trunk muscles, and pelvic floor muscles are best situated to work together to manage the downward pressure that happens both when you produce force (push your body away from the ground) and absorb force (control your body as it approaches the ground).
Once you can find that position, you can train it in all kinds of movements from squats to deadlifts to kettlebell cleans to jumping. The more explosive the movement, the more difficult the pressure will be to control, so it’s important to start with the basics.
As you can see, strength training is a powerful tool to help promote pelvic health. If you have been struggling with pelvic floor symptoms or a pelvic health condition and have been told that strength training is off the table for you, it isn’t! There is a way to introduce it that decreases rather than increases pain, and teaches you how to better manage stress rather than over-stressing the system. I would encourage you to find a pelvic health provider that knows how to manage these variables so that you leave feeling stronger, healthier, and empowered.
Dr. Julia Rosenthal, DPT, OCS, PRPC treats patients with all pelvic health and orthopedic conditions, and sees these elements of her practice as inextricably linked. Her approach integrates hands-on techniques with movement, exercise, and loading. Whether you’re living with chronic pain or experiencing pelvic floor dysfunction, no symptom or question is off-limits. She believes that physical therapy is about helping patients identify their values and goals, and providing individualized care that helps them take charge of their lives.

