My Journey With Vestibulodynia as a Patient and Clinician
By Jillian Giannini
PT, DPT
Have you heard of Vulvodynia, Vaginismus, or Vestibulodynia?
Well, in this blog, I’m going to focus on Vestibulodynia. I’m especially passionate about it because of my own personal journey experiencing it. It is key to understand this so that someone with this condition can find the right specialist and best possible treatment.
I’ve seen many patients come to our sessions with the diagnosis of Vaginismus or Vulvodynia when they may actually have Vestibulodynia, which may require us to gear their treatment in a different direction. Now, I’m not dismissing Vaginismus and Vulvodynia–I’ve had patients come in to see me for these conditions as well. However, when we do a deeper dive into someone’s story, their symptoms, and assess their vulvar tissues, we may find that it’s actually the vulvar vestibule that is contributing to their pain.
What is the difference between Vulvodynia, Vaginismus and Vestibulodynia?
Vaginismus: This is defined in the DSM-IV-TR as involuntary muscle spasms in the vagina that interferes with penetration. You may have also heard of Vaginismus falling under genito-pelvic pain/penetration disorder.¹
Vulvodynia: “Vulvar pain of at least 3 months’ duration, without clear identifiable cause, which may have potential associated factors”. The pain can be provoked, (i.e. with contact, penetration), spontaneous, or mixed. This can be pain anywhere in the vulva, which consists of the mons pubis, labia majora and minora, clitoris, vulvar vestibule, glands, urethral and vaginal opening.² To learn more about the various subsets and associated factors, refer to the 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia paper.
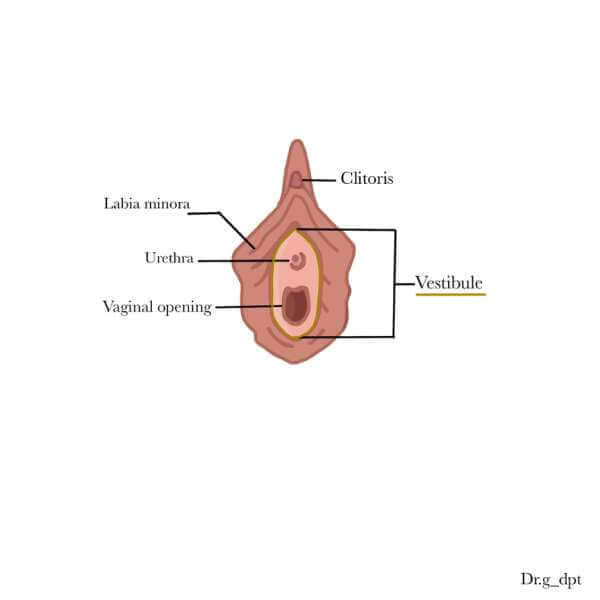
Vestibulodynia: A subset of Vulvodynia. It is pain localized specifically at the vulvar vestibule, which is the tissue around the vaginal entrance enclosing the urethral opening, vaginal opening, greater and lesser vestibular glands. You can see this tissue starting underneath the clitoris and on the inside of the labia minoras. This can also be provoked (i.e. with touch, penetration). Refer to this simple drawing I did, highlighting the vestibule:
People can have a combination of these diagnoses, like having both Vestibulodynia and Vulvodynia. Or they may just have Vaginismus, and not have Vulvodynia or Vestibulodynia. But for the purposes of this blog, I’m going to just focus on Provoked Vestibulodynia, which is provoked pain localized to the vestibule.
I was experiencing this in physical therapy school and had no idea what was going on. It wasn’t until I got into the field of pelvic health physical therapy that everything started to come together. When I was in physical therapy school, I started to notice I was having pain at the vaginal opening every time I had sex and gynecological exams. This started to just progressively get worse to the point where digit insertion and tampon use began to be painful as well. I felt like my tissues were raw, stinging, like they were about to rip. Not fun!
I felt like I was constantly in and out of gynecologist’s offices. One response I got was, “you’re just stressed with physical therapy school”. This was so frustrating to hear because, what was I supposed to do? Just wait 3 years?
When I started working in pelvic health physical therapy, I started to see patients with similar stories to mine and I started to learn the various potential causes and treatments. As pelvic health physical therapists, we work closely with various doctors since a lot of the time, treatment requires more than just physical therapy but more of a multidisciplinary approach.
So, I went to see one of the doctors we refer to that specializes in sexual medicine. In our appointment she assessed my vulvar tissues, looking for any redness, irritation, or signs of hormonal changes. She also performed a cotton swab test. If you’re unsure of what this test is, check out this instagram post I did explaining how I perform it. During this examination I didn’t have any pain when she pressed on the external parts of the vulva, but when she started to press along the vestibule, it was game over. It was definitely a pain in my hoo-ha!. She completely replicated the pain I was feeling, and that was the first time I felt validated.
Possible causes and “potential associated factors” for Provoked Vestibulodynia:
- Decreased hormones (ie: hormonal contraceptives, spironolactone)
- Overactive/hypertonic pelvic floor muscle dysfunction
- Too many nerve endings
- Inflammation (ie: chronic infections, vaginitis)
- Irritant/Allergen exposure
It’s actually quite exciting to see that we are starting to learn more about potential associated factors to this diagnosis. We still have a lot to learn and more research is still needed, but the more we know, the better treatments we can have for Provoked Vestibulodynia.
A lot of the time, a multitude of these factors can be happening together. For instance, we can see overactive or hypertonic pelvic floor muscles in conjunction with decreased hormones. This is what happened in my scenario. I have a long history of hormonal contraceptive use. My lab tests showed I had high Sex Hormone Binding Globulin levels and low free testosterone and I also had pelvic floor dysfunction. I just want to clarify, this doesn’t happen to everyone that uses hormonal contraception, but it’s important to be aware of it just in case you experience symptoms like painful sex.
What does Treatment look like?
The treatment will be dictated on what may be the associated factors to the Provoked Vestibulodynia. In my case, because decreased hormones were suspected and the vulvar vestibule is dependent on androgens, my treatment consisted of a localized hormonal topical to be applied to the vestibule along with pelvic health physical therapy. Again depending on what may be contributing, other forms of treatment may include oral medication (ie: nystatin, singulair), topicals (ie: gabapentin cream), or surgery (vulvar vestibulectomy).
Just like many other diagnoses associated with pelvic pain, it really is a journey, and what’s so important is finding a supportive and multidisciplinary team. My role as a pelvic health physical therapist is to help treat the musculoskeletal component that can be contributing to this, and being able to know when to refer and work with the right specialists to provide the best care for my patients.
I’m happy to say that I am now experiencing pain free sex and gynecological exams, but it took me some time to get here with lots of ups and downs. Everyone’s journey and path is different, but I hope I am able to at least share some knowledge that I wish I had sooner and help guide you to the resources you may need.
To access specialists who treat Vestibulodynia, check out the International Society for the Study of Women’s Sexual Health (ISSWSH) and International Society for the Study of Vulvovaginal Disease (ISSVD) to access their directories.
References:
- Lahaie MA, Boyer SC, Amsel R, Khalifé S, Binik YM. Vaginismus: a review of the literature on the classification/diagnosis, etiology and treatment. Womens Health (Lond). 2010 Sep;6(5):705-19. doi: 10.2217/whe.10.46. PMID: 20887170.
- Bornstein J, Goldstein AT, Stockdale CK, Bergeron S, Pukall C, Zolnoun D, Coady D; consensus vulvar pain terminology committee of the International Society for the Study of Vulvovaginal Disease (ISSVD); International Society for the Study of Women’s Sexual Health (ISSWSH); International Pelvic Pain Society (IPPS). 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. J Sex Med. 2016 Apr;13(4):607-12. doi: 10.1016/j.jsxm.2016.02.167. Epub 2016 Mar 25. PMID: 27045260.
Jillian Giannini, PT, DPT is the owner of LIA Pelvic Health and is a pelvic health physical therapist in Los Angeles, CA. She works with all genders who are experiencing bladder, bowel and sexual dysfunction. She treats the whole person and takes on a holistic approach with her patients. Her passion lies in educating and spreading the word about pelvic health physical therapy so people can find the help they need.

