Painful Sex Can Go Away: Here’s What You Need to Know
By Julie Sarton
PT, DPT, WCS
Scope of the Problem
Painful sex is more common than you think. Studies indicate anywhere from 25-60% of women will experience sexual pain at some point in their life. (Trahan 2019). Painful sex (also known as Dyspareunia) can cut across the entire lifespan. In fact, 9/10 women will experience pain the first time they have sex after baby. 45% of women experience pain 3 months after baby arrives and at 18 months postpartum, 23% of women still have sexual pain.
What about as women age? The literature reveals that between 20-30% of all menopausal women report sexual difficulties and sexual pain. If we look at the breast cancer population, we find that up to 70% of women report sexual pain.
With these statistics being so high, why are most providers not educated better on how to truly treat this common but not normal problem so many women face? According to a study by Cherpak in 2016, 63.9% of MDs do not address sexuality in medical interviews.
The 3 top reasons for this were found to be:
1. Lack of time
2. Fear of embarrassment
3. Inability to address the issue
When women suffering with sexual pain do talk, they unfortunately are often told the wrong thing or dismissed by their health care professional. Read some of the comments that have been shared in our clinic over the last 25 years.
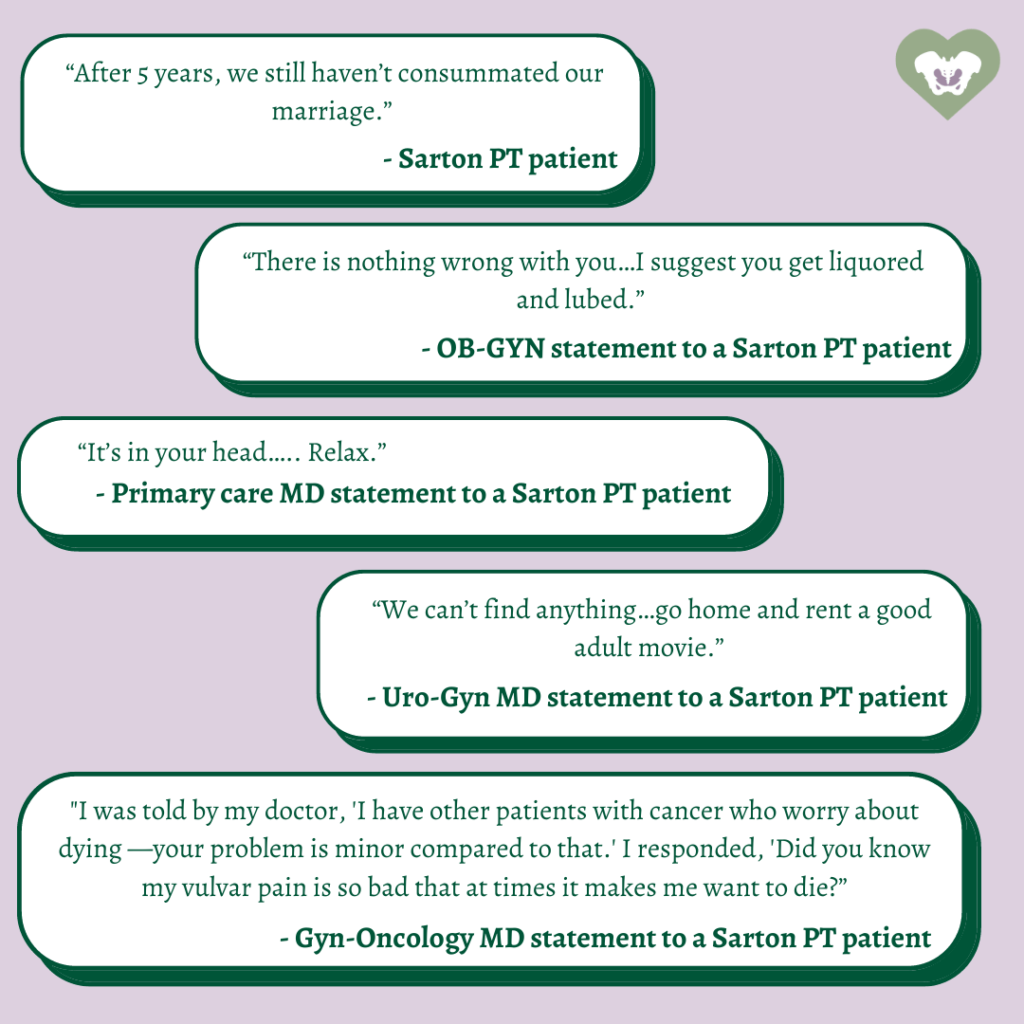
Statements like the ones highlighted above are unacceptable and truly have no place in medicine. In order to help change this, we need to equip MDs/NPs/PTs/OTs who treat this as well as patients who suffer with painful sex with better, more accurate and up to date information.

Causes of Sexual Pain
Sexual pain can stem from a variety of reasons. Underlying drivers can range from issues with hormones, to issues with the pelvic floor muscles (a hypertonic pelvic floor) to issues with nerve endings in the vulva, clitoris or perineum or even be due to skin changes from inflammation or dermatological issues like Lichen Sclerosus. One of the most common diagnoses we see in our clinic driving sexual pain that is often missed is something known as vestibulodynia. Vestibulodynia is a subcategory or type of vulvodynia.
What is Vulvodynia and Vestibulodynia?
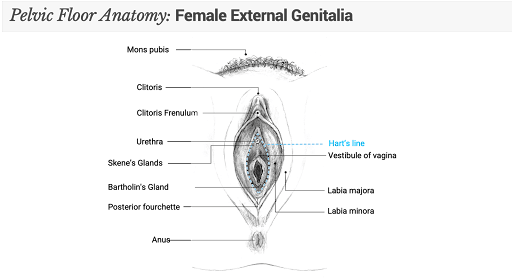
The term vulvodynia has been used as a diagnosis for years, however when we break down the meaning of the word we see vulvodynia is a “symptom” rather than a diagnosis – it literally means pain (dynia) in the vulvar region (vulvo). It is used to describe the symptoms of chronic or recurrent pain and discomfort in the vulvar region resulting in pain with sex. If you are like most women, you might not understand exactly what your vulva is and what structures this includes. All you know is that you have pain “down there” and this is not normal. Essentially, the vulva includes the following: the mons pubis, the clitoris, the labia majora, labia minora, the vulvar vestibule, the urethral opening, the vaginal opening, and Bartholin’s and Skene’s glands. See Figure 1 for Vulvar anatomy.
Women with vulvodynia can have pain that is provoked (such as pain due to intercourse, pain with sitting, wiping after urination, wearing underwear, undergoing an annual exam or tampon insertion), or pain can be unprovoked (pain surfacing without any type of touch, clothing or specific activity). Another important factor to note is that pain can be generalized to the entire vulva, or limited to just one area, such as the vestibule or clitoris.
When the pain and symptoms are limited to the vestibule, this is known as vestibulodynia. Vestibulodynia is the most common form of vulvodynia and a frequent reason why a lot of women experience entrance dyspareunia (pain with penetration during intercourse attempts). For a detailed article on vestibulodynia, please refer to Hartmann and Sarton’s article (Hartmann D, Sarton J, Chronic pelvic floor dysfunction, Best Practice & Research Clinical Obstetrics and Gynaecology (2014).
Manifestations of Vestibulodynia
The nature of vestibulodynia may vary widely from woman to woman. Symptoms can include burning, rawness, searing, stinging or a sharp pain in the vestibule or entrance to the vagina. The pain can be constant, intermittent, or only occurring when the vulva is touched, as mentioned above.
Common descriptors include:
- Pain inside the labia minora at the entrance to the vaginal opening
- Uncomfortable tingling and/or burning sensations in the vestibule
- Stinging, itching, or raw feeling in vulvar tissue
- Throbbing, aching, soreness, and swelling
- Redness may or may not be present
- Involvement of the urethral opening may lead to symptoms resembling a Urinary Tract Infection (urgency and/or frequency, pain with urination)
- Hyperalgesia—increased response to stimulus that normally is painful
- Entrance Dyspareunia—painful penetration with intercourse
- Pelvic floor muscle hypertonicity of superficial and deep (present in 90% of patients)
- Light touch triggers pain = allodynia. Tight pants, undergarments, and movement of pubic hair may provoke discomfort and pain.
Phenotypes of Vestibulodynia
Thankfully, we have come a long way with our understanding of what sets the stage for vulvodynia and vestibulodynia. Recall that the term ‘vulvodynia’ simply means pain in the vulva—it truly is not a diagnosis, but rather a descriptor of what is happening. This is a label that only tells you that pain is present in the vulva—similar to saying you have “knee pain.”
WE NOW RECOGNIZE THAT THERE ARE DISTINCT ETIOLOGIES OF VESTIBULODYNIA (AND WHILE MANY OF THESE ETIOLOGIES OVERLAP), IT IS ESSENTIAL TO RECOGNIZE THE DISTINCT COMPONENT OF THIS SYNDROME.
This relevant categorization outlines phenotypes of vestibulodynia, taking into account what the various underlying causes are.
Please refer to Figure 2 below:

Depending upon the person, which phenotype, the location of pain, the constancy, the severity and the underlying perpetuating factors, symptoms and treatment will vary.
Therefore, each treatment plan will need to be unique!
Recent literature further links associations between vulvodynia/vestibulodynia and fibromyalgia, chronic fatigue syndrome, yeast infections, recurrent vulvovaginal infections, irritable bowel syndrome, interstitial cystitis and oral contraceptive use.
Therefore, your healing team of practitioners will need to almost always involve a multi-disciplinarian team. Often, a pelvic floor therapist serves as a primary player on this healing team, as PTs and OTs tend to spend more time with you than most other practitioners (Note: find a facility that offers at least 1 hour treatments!) You can rest assured knowing that an experienced PT or OT will help you manage your case, and then refer/collaborate with other team members as needed.
Hypertonic Pelvic Floor Muscle Dysfunction as a Phenotype of Vestibulodynia or Vulvodynia
Increased muscle tone causes a decrease in blood flow and oxygen to the muscles of the pelvic floor. This can lead to a build up of lactic acid. Symptoms of pelvic floor muscle hypertonicity include: generalized vulvar pain or burning, tenderness where the muscle insert in front of and behind (4, 6, and 8 o’clock) the vestibule which causes severe introital dyspareunia (pain with sex), urinary symptoms (frequency, hesitancy, incomplete emptying), constipation, hemorrhoids, and rectal fissures. Physical exam may or may not reveal erythema where the muscles insert at the vestibule, multiple pelvic floor muscular trigger points, muscles weakness, and an inability to hold a sustained contraction.
How Does Pelvic Floor Therapy Help Specifically?
Pelvic floor physical therapy is not new, and pelvic floor muscle hypertonicity was first implicated back in the mid-1990s as a trigger of major chronic vulvar pain. The early studies revealed that hypertonic PFMs (pelvic floor muscles) were successfully treated using surface electromyography or biofeedback, and complaints of vulvar pain and sexual dysfunction were decreased (Hartmann, Sarton 2014).
Today, pelvic floor physical therapists offer a much more comprehensive approach to the management of chronic vulvar and pelvic pain.
As pelvic health specialists who have received extensive education in the treatment of chronic pelvic dysfunction, we can offer an array of highly specialized manual therapy techniques to treat vulvodynia, vestibulodynia, and all the comorbid conditions that are commonly seen with it. Musculoskeletal, fascial, nerve and visceral aspects should always be evaluated and treated with any and each patient. Your pelvic therapist will perform an extensive external and internal evaluation to determine which of over the 30 muscles attaching into the pelvis are part of the problem. If the pelvic floor muscles are found to be hypertonic, it is your therapist’s job to figure out if the PFMs are the driver of pain or the victim of something else going on.
Summary
Vestibuldoynia – a common cause of painful sex- CAN BE HELPED via multi-modal therapy, with pelvic floor PT being a key essential component to treatment (Hartmann D, Sarton J, Chronic pelvic floor dysfunction, Best Practice & Research Clinical Obstetrics and Gynecology 2014). It is critical to put together a multidisciplinary team to address and resolve your sexual pain Find a highly skilled pelvic floor therapist who routinely treats vestibulodynia-hope and healing are possible and you will be taking 1 step closer to recovery!
Dr. Julie Sarton is among the nation’s foremost experts on the pelvic floor. She founded Sarton Physical Therapy in 2011 with the vision to provide hope and healing to patients from all over the world with the best possible staff and evidence-based treatment. The clinic has grown rapidly, treating patients from across the country and even internationally.

