Role of OT in Men’s Pelvic Health
By Lainie Givens
OTR/L, CPHS
As we attempt to put more of a spotlight on men’s pelvic health, it is important to note different specialists equipped to treat men’s pelvic health issues. Although not as widely acknowledged as physical therapy in the realm of treating pelvic floor dysfunction, occupational therapy is equally—if not greater—proficient to focus on pelvic health, particularly men’s pelvic health. What, you ask, is occupational therapy?
According to the American Occupational Therapy Association, occupational therapy “uses everyday life activities (occupations) to promote health, well-being and your ability to participate in the important activities in your life”. Occupations range from things like dressing, urinating, having a bowel movement, and sexual function to walking your dog, bike riding and making a meal for your family. Life can interfere with these occupations in a variety of ways, including surgery, pain, injury, or stress just to name a few. Occupational therapists are trained in taking a holistic approach, looking at physical, psychological, emotional and social factors to determine appropriate treatment. They incorporate all of these factors into treatment as necessary. Occupational therapy focuses on function, quality of life, and meaning for each individual. So how is this related to men’s pelvic health?
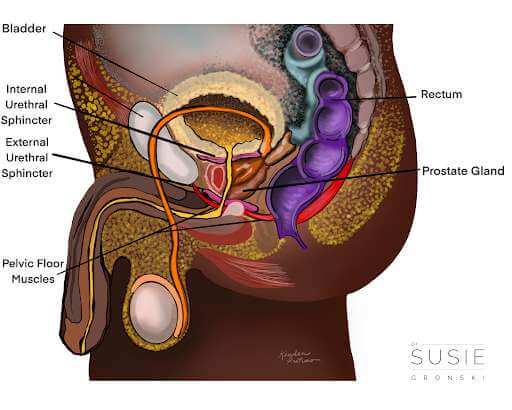
The pelvic floor is a group of muscles and tissues that create a hammock which supports the internal organs including the bladder, urethra and prostate, prevents leakage of urine and feces, and aids in sexual function.
Men’s pelvic health encompasses a variety of topics including but not limited to pelvic pain, genital pain, erectile dysfunction, difficulty urinating, constipation, sexual pain, and surgery. Several of these (peeing, pooping and sex!) are Activities of Daily Living (ADLs) which occupational therapists are specialized in treating. Additionally, while these issues may appear strictly physical, research shows they can be multifactorial. A research study conducted in 2022 found that anxiety, depression and relational conflicts can both cause and affect sexual dysfunction. Erectile difficulty or dysfunction also has both psychological and physical sources, with the parasympathetic nervous system controlling the erection process and sympathetic controlling the ejaculatory process. Knowing that the pelvic floor components and processes are modulated and affected by responses from brain and body tells us that treatment should encompass both. Occupational therapists are trained to identify and treat these components.
Pelvic floor muscle function is important to evaluate if you have encountered one of the above pelvic health issues. In pelvic floor OT, you will receive a thorough physical exam including an external and internal exam of the pelvic floor and genitals and an evaluation of how your body moves functionally. This will help determine the needs of the musculature in the pelvis, and allow us to assess pelvic floor muscle coordination both in isolation and during movement. We will also discuss things like habits, routines, roles and stress level, which, from an occupational therapy perspective, are of equally important impact. Habits, routines and roles help establish lifestyles and can support or hinder occupations.
Occupational therapists help to create, modify, and adapt habits and routines to support sexual function, bladder and bowel function, or being pain free during preferred activities and exercise. Have you ever thought about how your bladder or bowel habits affect your day, or your pain? Or how your work schedule affects your bowel/bladder routine? Or maybe how your masturbation routine (gasp!) affects your ability to engage in sexual intercourse with a partner in the way you want to? I challenge you to recall a daily habit or routine that impacts another or maybe multiple other areas of your life. A recent research study concluded that distress related to pelvic floor dysfunction is correlated with quality of life more so than muscle function. This is further evidence that it is imperative to tackle all aspects affecting pelvic floor dysfunction, and highlights why occupational therapists are well equipped to treat men’s pelvic health.
Through education, activities and exercise, occupational therapists help people regain function in the pelvic region. This could mean exercises targeted toward a specific movement of rock climbing, controlling incontinence after a prostatectomy, or determining what seat or adaptive cushion works best for your long bike rides after suffering from pelvic pain. OT can help you identify the root(s) of your ailment and collaboratively develop a plan for healing.
Curious about the optimal time to consult a pelvic health occupational therapist?
A pelvic health occupational therapist can provide valuable assistance in managing the following:
- Pelvic Pain
- Erectile Difficulty
- Urinary or Bowel Leakage
- Sexual Dysfunction or Pain
- Surgery – pre and/or post-op for any abdominal or pelvic procedure including hernia repair and prostatectomy
- Sensation changes in the pelvic region or genitals
- Any change “down there” that is affecting your ability to engage in what is meaningful to you
Lainie is a Licensed Occupational Therapist and Certified Pelvic Health Specialist at Dr. Susie Gronski, Inc. in Asheville, NC. She specializes in promoting health and independence in important daily activities such as bowel movements, urination, and sexual intimacy. Through person-centric strategies, Lainie blends therapeutic recreation with occupational therapy to support individuals facing illnesses or disabilities, aiming to enhance their overall well-being and quality of life.
References:
- Occupational Therapy Practice Framework: Domain and Process, Fourth Edition
- https://www.aota.org/about/what-is-ot
- https://www.ncbi.nlm.nih.gov/books/NBK513278/#:~:text=Engorgement%20of%20the%20corpus%20spongiosum,during%20the%20rigid%20erection%20phase.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9326597/#:~:text=Anxiety%2C%20depression%2C%20and%20relational%20conflicts,cause%20and%20affect%20sexual%20dysfunction.
- https://pubmed.ncbi.nlm.nih.gov/32915304/
https://www.continence.org.au/who-it-affects/men/male-pelvic-floor-muscles

